Neurofibromatosis (NF) is a genetic disorder of the nervous system which causes tumors to form on the nerves anywhere in the body at any time. This progressive disorder affects all races, all ethnic groups and both sexes equally. NF is one of the most common genetic disorders in the United States (one in every 2,500 to 3,000 births). The neurofibromatoses affects more than 120,000 Americans.
NF has three genetically distinct forms: NF-1, NF-2 and Schwannomatosis. They are caused by different genes and chromosomes. The effects of NF are unpredictable and have varying manifestations and degrees of severity. There is no known cure for any form of NF, although the genes for both NF-1 and NF-2 have been identified.
NF is an autosomal dominant genetic condition; it is not contagious. Approximately 50% of those affected with Neurofibromatosis have a prior family history of NF. The other 50% of cases are the result of spontaneous genetic mutation. If an individual does not have NF, s/he can not pass it on to his/her children.
Neurofibromatosis causes unchecked growth of tissue along the nerves. This can put pressure on affected nerves and cause pain, severe nerve damage, and loss of function in the area served by the nerve. Problems with sensation or movement can occur, depending on the nerves affected. The condition can be very different from person to person, even among people in the same family who have the NF1 gene. The “coffee-with-milk” (café-au-lait) spots are the hallmark symptom of Neurofibromatosis. Although many healthy people have 1 or 2 small café-au-lait spots, adults with 6 or more spots greater than 1.5 cm in diameter are likely to have Neurofibromatosis. In most people with the condition, these spots may be the only symptom.
Two or more of the following: Six or more café-au-lait spots 1.5 cm or larger in post-pubertal individuals, 0.5 cm or larger in pre-pubertal individuals Two or more neurofibromas of any type or one or more plexiform neurofibroma Freckling in the axilla or groin Optic glioma (tumor of the optic pathway) Two or more Lisch nodules (benign iris hamartomas) A distinctive bony lesion: dysplasia of the sphenoid bone or dysplasia or thinning of long bone cortex A first-degree relative with NF1
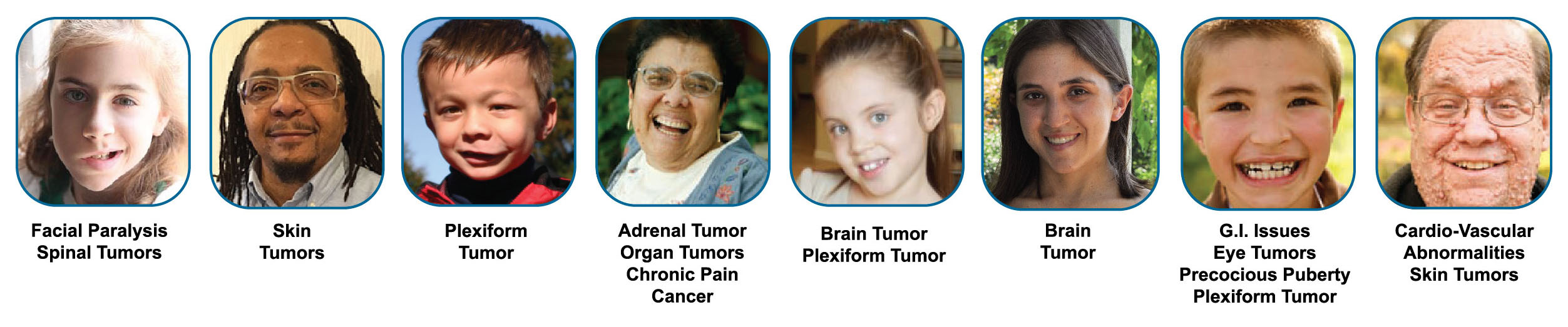
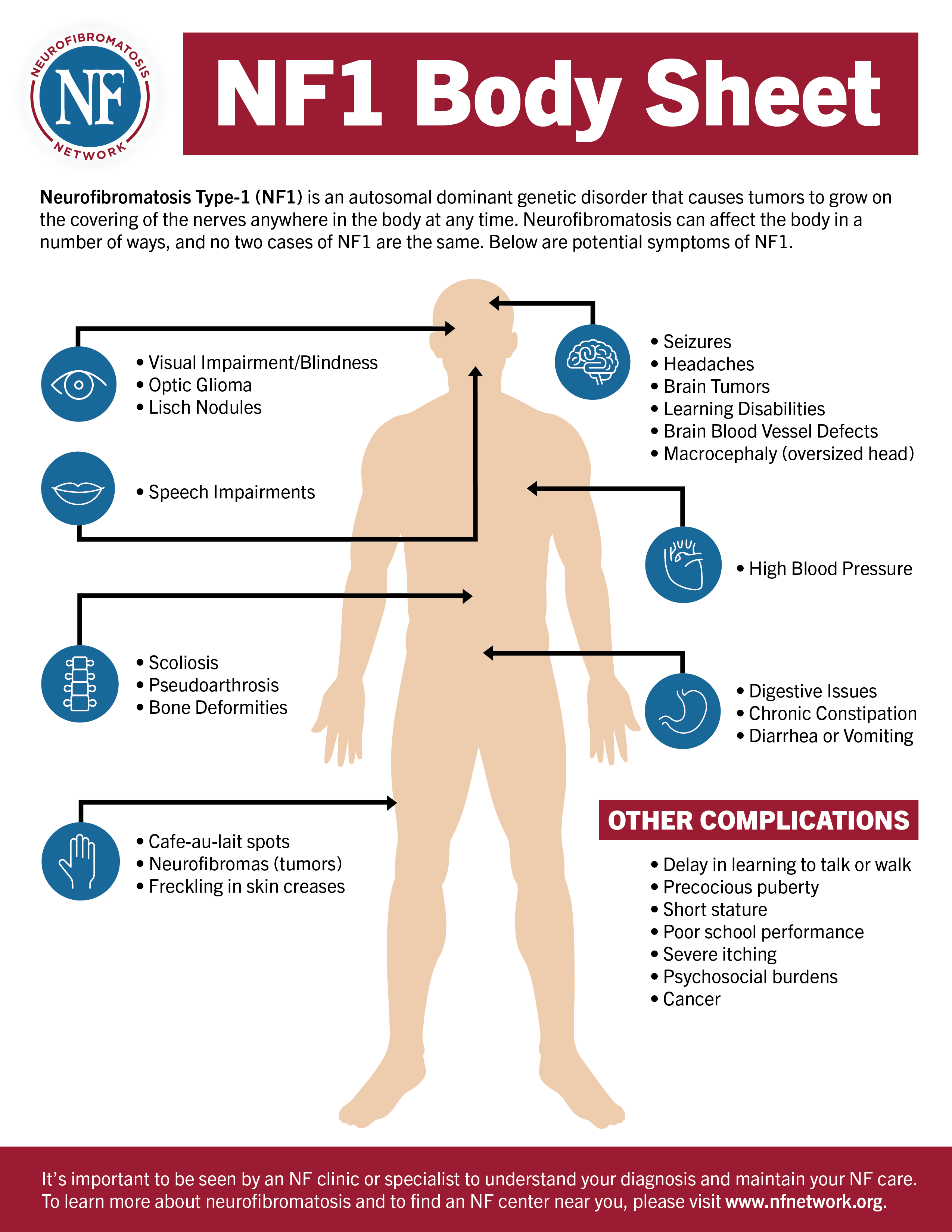
Neurofibromatosis type 1 (NF-1) is an autosomal dominant genetic disorder that causes tumors to grow on the covering of the nerves anywhere in the body at any time. The disorder affects 1 in 2,500 to 3,000 males and females of all races and ethnic groups. The NF-1 gene is located on chromosome 17. Other symptoms may include:
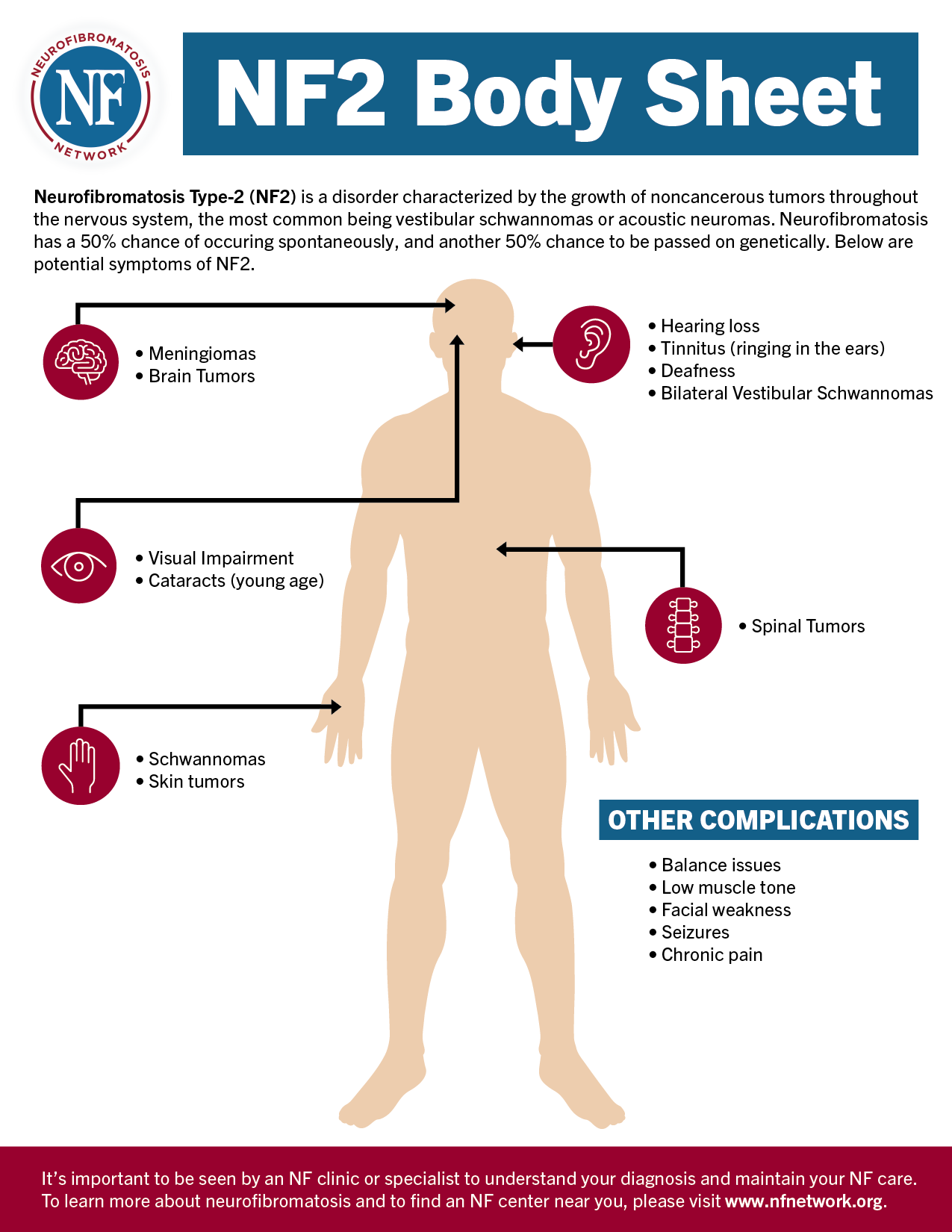
Neurofibromatosis type 2 (NF 2) is a disorder characterized by the growth of noncancerous tumors throughout the nervous system. The most common tumors associated with Neurofibromatosis type 2 are called vestibular schwannomas or acoustic neuromas. These are benign, usually slow-growing tumors that develop from the balance and hearing nerves supplying the inner ear.
If tumors develop in other parts of the brain or spinal cord, signs and symptoms vary according to their location. Complications of tumor growth can include changes in vision or sensation, numbness or weakness in the arms or legs, and fluid buildup in the brain. Many people with NF2 have posterior sub capsular cataracts in one or both eyes, often beginning in childhood.
NF2 can cause deafness, severe balance problems, facial nerve paralysis, spinal cord compression, swallowing difficulties and/or eye function complications. Autosomal dominant disorders, approximately 50% of the cases are inherited. This means that if one parent has NF2, any child of that parent has a 50-50 chance of having it. The other 50% of the cases are accounted for by a new mutation.
Neurofibromatosis 2 (NF 2) is distinguished by multiple brain and spinal tumors that can cause deafness, severe balance problems, facial nerve paralysis, spinal cord compression, swallowing difficulties or eye function complications. Neurofibromatosis 1 and Neurofibromatosis 2, share the same name, but are very different disorders
Although NF-2 is an autosomal inherited disease, it is also important to understand that 50% of the cases are “sporadic” - meaning it does NOT have to be inherited to originate.
Confirmed (definite) NF2:
Presumptive (probable) NF2:
Neurofibromatosis type 2 (NF 2) is an autosomal dominant genetic disorder that causes tumors to form on the nerves of the central nervous system, in the brain, and on the spine. It affects one in 25,000 males and females of all races and ethnic groups. The NF 2 gene is located on chromosome 22.
Schwannomatosis is estimated to occur in 1 in 40,000 births. The inheritance pattern of Schwannomatosis is not well understood. The risk of transmitting the disorder to offspring is about 15%. Schwannomatosis symptoms usually first appear in adulthood.
Schwannomatosis is characterized by:
Anyone with schwannomatosis experiences some degree of pain, but the intensity varies. A small number of people have such mild pain that they are never diagnosed with the disorder. Most people have significant pain, which can be managed with medications or surgery. In some extreme cases, pain will be so severe and disabling it will keep people from working or leaving the house.
There is no currently accepted medical treatment or drug for schwannomatosis, but surgical management is often effective. Pain usually subsides when tumors are removed completely, although it may recur should new tumors form. When surgery isn’t possible, ongoing monitoring and management of pain in a multidisciplinary pain clinic is advisable.